Minimally Invasive Back Pain Treatment in Marietta: What Are Your Options?
Back pain has a way of shrinking your world. In Marietta, it can show up the moment you sit down for the commute, climb into the car after a long day, or try to get through a grocery run without needing to lean on the cart. It’s the ache that makes you hesitate before picking up a child, the pinch that flares when you carry laundry up the stairs, and the stiffness that turns “standing at the stove” into something you dread instead of a normal part of your evening.
If that sounds familiar, here’s the reassuring truth: many causes of back pain can improve with modern, minimally invasive care. You do not have to jump straight to major surgery to get meaningful relief—and you don’t have to rely on stronger and stronger medications to get through the day.
At Medici Orthopaedics & Spine, our philosophy is straightforward: use the least invasive, least drug-dependent path that gives you the best chance at restoring function and quality of life.
If you’re in Marietta and back pain is interfering with work, sleep, movement, or family life, a modern evaluation can help clarify what’s going on and what your least invasive options truly are—so you can start moving forward with confidence instead of guessing.
Your Non-Surgical, Minimally Invasive Options in Marietta
Physical Therapy and Movement-Based Rehabilitation
Core Stabilization, Hip Mobility, Posture Training
This isn’t about doing endless crunches or forcing perfect posture. It’s about building:
- core endurance that protects the spine,
- hip mobility so the back doesn’t compensate,
- movement strategies that reduce flare-ups during bending, lifting, and sitting.
Graded Return to Activity (Avoid Boom/Bust Cycles)
A common trap is doing too much on a good day, then paying for it for three days. A graded plan rebuilds tolerance without constantly poking the bear.
Functional Milestones: Walking, Standing, Lifting, Stairs
A good plan measures progress in what you care about:
- standing through a shift,
- lifting groceries without fear,
- taking stairs comfortably,
- walking farther without needing breaks.
Lifestyle and Ergonomics That Reduce Flare-Ups
Safe Lifting Basics and Workstation Setup
Whether you’re lifting kids, moving boxes, or working at a desk, basics matter:
- how you hinge and brace,
- how long you sit without breaks,
- where your monitor and chair support are positioned.
Weight Management and Anti-Inflammatory Habits
If weight, inflammation, or conditioning are contributing, the goal is never shame—it’s leverage. Even modest improvements in strength, walking tolerance, and daily movement can decrease load on pain-sensitive structures.
Sleep Positioning and Recovery Strategies
Back pain and poor sleep feed each other. Simple adjustments—pillow support, position changes, a consistent wind-down routine—can reduce nighttime flare-ups and help your body recover.
Medication Management
When Meds Are Appropriate
Short-term medication strategies may be useful during acute flare-ups or while inflammation is being calmed so you can participate in rehab.
Avoiding Unnecessary Dependency and Excessive Sedation
Many people don’t realize how much some medications can affect:
- alertness,
- balance,
- reaction time,
- sleep quality.
Interventional Spine Treatments: Targeted Relief Without Major Surgery
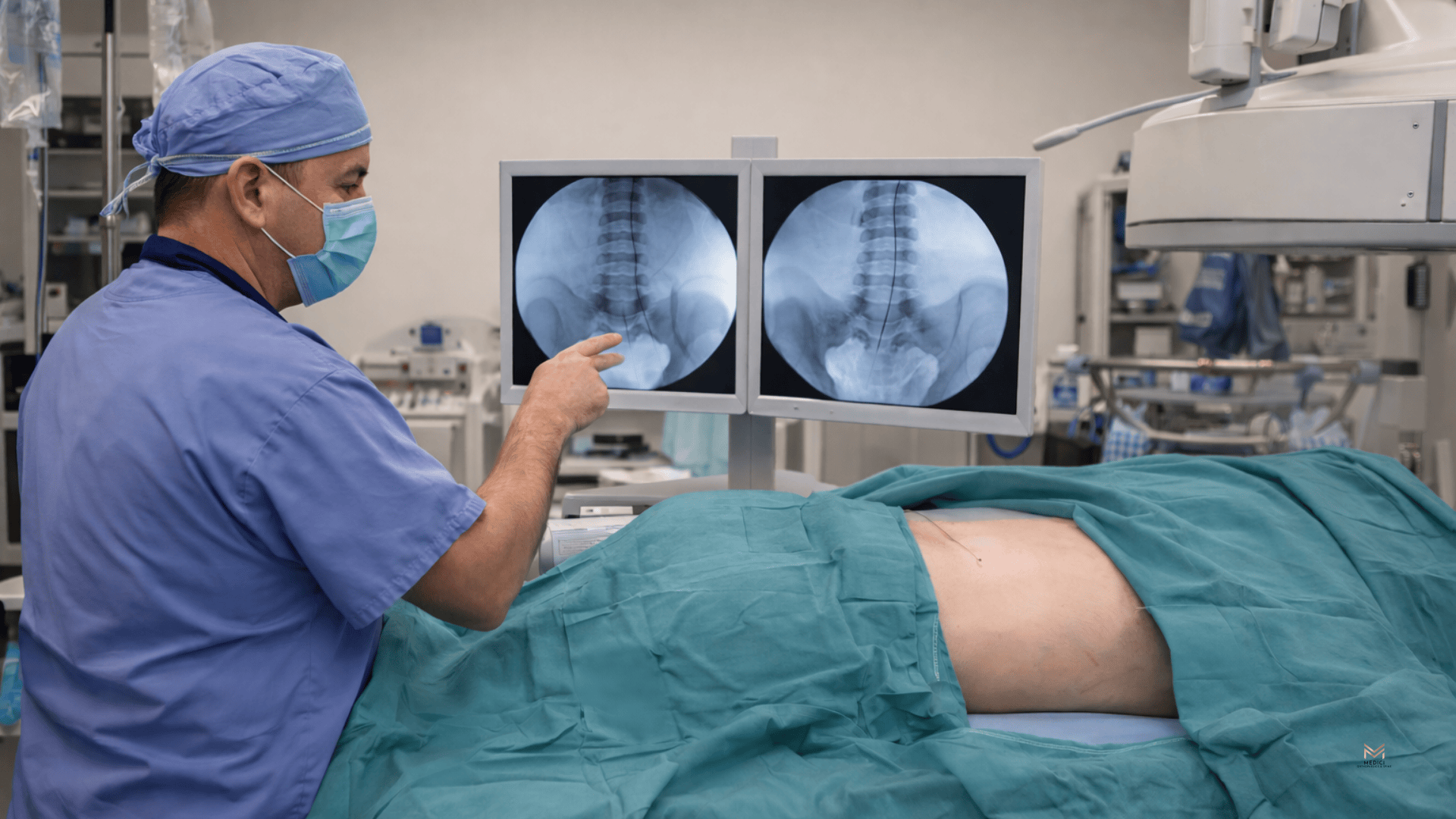
Image-Guided Epidural Steroid Injections
When They’re Used
Epidural injections are commonly considered when symptoms suggest:
- disc-related nerve irritation,
- sciatica-like pain,
- inflammation from stenosis that limits walking/standing.
What They Can Help
These treatments are often most effective for radiating leg pain and nerve-driven symptoms. In some cases, back pain improves too—especially if inflammation is a major driver.
What to Expect
These are typically performed with imaging guidance for accuracy. Many patients return to light activity quickly, and relief may be gradual as inflammation settles. The goal is often to create a window where rehab and normal movement become possible again.
Facet Joint Injections and Medial Branch Blocks
Who May Benefit
If your pattern matches facet-driven pain, targeted injections or diagnostic blocks can help confirm the source and reduce symptoms.
Diagnostic vs. Therapeutic Role
Medial branch blocks are often used diagnostically—to confirm whether the facet joint nerves are the true pain generator—so next steps are more confident and precise.
Radiofrequency Ablation (RFA)
What It Is
RFA uses heat to disrupt pain signals from specific nerves that supply the facet joints. It does not “fix arthritis,” but it can significantly reduce pain for the right candidates.
How Candidacy Is Determined
Typically, the best predictor of success is a strong response to diagnostic medial branch blocks.
Expected Duration of Relief
Relief varies by person, but it’s often measured in months, not days—helping many patients return to activity, rehab, and daily life with less limitation.
SI Joint Injections
For SI Joint-Driven Pain Patterns
If the exam suggests the SI joint is the source, an injection can reduce inflammation and confirm the diagnosis.
How They Fit Into Rehab Planning
The injection isn’t the finish line—it’s often a tool to reduce pain enough to strengthen and stabilize the area so symptoms don’t keep cycling back.
Trigger Point Injections and Myofascial Treatments
When Muscle/Fascia Are Major Contributors
Myofascial pain can create deep aching, tight bands, and referral patterns that feel like “back problems” but respond best to targeted muscular treatment.
Pairing With PT for Longer-Term Results
Trigger point treatments can reduce pain and guarding, but pairing them with rehab is what helps create lasting change—better movement, better endurance, fewer flare-ups.
Regenerative Medicine and Supportive Therapies
Platelet-Rich Plasma (PRP) Injections
PRP uses a concentrated portion of your own blood (platelets and growth factors) that’s injected into a targeted area to support healing and reduce inflammation.
Where PRP may fit (selected cases):
- certain facet joint pain patterns
- certain SI joint pain patterns
- tendon/ligament irritation around the low back/pelvis (support structures that can contribute to instability-like pain)
Prolotherapy
Prolotherapy involves injecting an irritant solution (commonly dextrose-based) into painful ligaments/tendon attachments to stimulate a healing response and improve tissue support over time.
Where prolotherapy may fit (selected cases):
- ligament laxity or chronic sprain-like pain around the pelvis/low back
- some SI joint-related pain patterns
- supportive care when instability or “giving way” sensations are part of the story
Complementary Therapies That Can Help Function
Myofascial Release and Sports Massage Therapy
If muscle guarding and fascia tightness are major drivers, techniques like myofascial release or sports massage can help:
- reduce protective tightness,
- improve mobility,
- make it easier to participate in rehab exercises,
- and decrease the “stuck” feeling that keeps you moving cautiously.
Hyperbaric Oxygen Therapy
Hyperbaric oxygen therapy may be considered in specific circumstances where improving tissue oxygenation and supporting recovery is clinically appropriate. It’s not a routine first-line treatment for everyday back pain, but in the right context, it may be discussed as part of a broader, carefully selected care plan.
Advanced Options for Chronic Back and Nerve Pain
Spinal Cord Stimulation (SCS)
What It Is
SCS is a form of neuromodulation—a therapy designed to change how pain signals are processed so the nervous system doesn’t keep amplifying them.
Who May Benefit
SCS is typically considered when:
- pain has persisted despite reasonable conservative and interventional care,
- symptoms significantly affect sleep and daily function,
- and the clinical picture fits the type of pain SCS is designed to address.
Trial Process Before Long-Term Placement
One of the most patient-friendly aspects of SCS is that it typically involves a trial first. That means you can assess how much it helps before making any long-term decisions.
Functional Goals Often Targeted
Success isn’t just “a lower number on a pain scale.” Many people are aiming for:
- better sleep,
- improved walking tolerance,
- more consistent daily activity,
- fewer flare-ups and less fear of movement.
Start With the Least Invasive Path to Back Pain Relief in Marietta
You don’t have to accept ongoing back pain as “normal”—especially when it’s stealing your sleep, making work harder, or limiting your mobility. The longer pain lingers, the more it can affect how you move, how you rest, and how confident you feel doing everyday things. But persistent back pain doesn’t automatically mean you need major surgery or a lifetime of medications.
Many patients improve without major surgery by identifying the true pain generator and choosing modern, targeted treatments that match it. When care is specific—disc-related pain vs. facet/SI joint-driven pain vs. nerve-related symptoms vs. muscular or myofascial contributors—results tend to be clearer, more predictable, and less invasive.
If you’re ready for answers, schedule an evaluation to determine whether your back pain is disc-related, facet or SI joint-driven, nerve-related, muscular, or a combination—and build a stepwise plan that prioritizes the least invasive option that can genuinely move you forward.
Contact Medici Orthopaedics & Spine
- Website: https://www.mediciortho.com/
- Main Phone: +1-844-328-4624
Marietta Ambulatory Surgery Center
792 Church Street, Unit 101
Marietta, GA 30060









